Vaccination has been a hot topic over the past year. When will they be ready? Are they safe? Are they effective?These are some of the pressing questions around COVID-19 vaccines, currently our best bet against protecting us from the novel Coronavirus. Once the vaccines were ready, however, enthusiasm towards getting inoculated was not as high as hoped. According to a recent poll by the Pew Research Center, only 60% of Americans planned to get a COVID-19 vaccine. To make matters worse, past research suggests that people who say they intend to get vaccinated are likely to not follow through. Experts have estimated that to reach herd immunity, 60–90% of Americans must be inoculated against the novel coronavirus but if those numbers aren’t reached then herd immunity remains a faraway dream. And the consequences of this are disastrous.
Once the vaccines were ready, however, enthusiasm towards getting inoculated was not as high as hoped. According to a recent poll by the Pew Research Center, only 60% of Americans planned to get a COVID-19 vaccine. To make matters worse, past research suggests that people who say they intend to get vaccinated are likely to not follow through. Experts have estimated that to reach herd immunity, 60–90% of Americans must be inoculated against the novel coronavirus but if those numbers aren’t reached then herd immunity remains a faraway dream. And the consequences of this are disastrous.
But is this issue with uptake intentions only the problem of vaccines for COVID-19? Unsurprisingly, it is not. The Centers for Disease Control and Prevention recommends that every American over 6 months of age receive a flu shot, because inoculation typically reduces the chances of contracting the flu by at least 50%. However, less than half of Americans were vaccinated during the 2019–2020 influenza season, which could have prevented tens of thousands of deaths by influenza during that period.

There are interesting parallels between uptake for the flu vaccine and uptake for the COVID-19 vaccine, that haven’t gone unnoticed with leading behavioral scientists. Katy Milkman, John Beshears and Dilip Soman among many other behavioral scientists conducted a large field experiment on boosting influenza vaccine uptake. And we do mean large, as it used 19 different nudge variations delivered to 47,306 people, randomly selected into one of the 19 conditions.
The study was conducted in the fall of 2020, in partnership with two large health systems in the North-eastern United States. Participants were part of one of those two health systems and had had new or routine (non-sick) primary care appointments between September and December 2020. Additional inclusion criteria included the patients had a cell phone number recorded in their electronic health record; they had not opted out of receiving SMS appointment reminders from their healthcare provider or asked not to be contacted for research purposes, they did not have a documented allergy or adverse reaction to the flu vaccine, and finally they had not received a flu shot in 2020 according to their electronic health record.
The 19 conditions were based on 19 different text messaging protocols. Protocols varied the tone (I.e., formal versus casual) as well as the timing of up to two sets of text reminders. The team got creative and constructed surprising, creative and even interactive nudges. For example, one of the most artful interventions featured a joke about spreading the flu as told by a dog or cat, in picture form, was among the interventions tested. Messages were sent from the patient’s healthcare provider to their phone in the 3 days preceding the patient’s appointment.
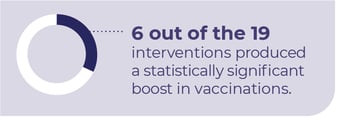 In the end, all of the 19 interventions directionally increased vaccination rates, the desired outcome variable, by an average of 2.1 percentage points. 6 out of the 19 interventions (32% of interventions) produced a statistically significant boost in vaccinations. The top-performing intervention showed a 4.6 percentage point boost in vaccination. What differentiated the top performer from other conditions?
In the end, all of the 19 interventions directionally increased vaccination rates, the desired outcome variable, by an average of 2.1 percentage points. 6 out of the 19 interventions (32% of interventions) produced a statistically significant boost in vaccinations. The top-performing intervention showed a 4.6 percentage point boost in vaccination. What differentiated the top performer from other conditions?
The top-performing condition relied on two messages being sent to the patient. The first text message in this condition was sent 72 hours before the patient’s appointment and it stated that, “it’s flu season, a flu vaccine is available for you.” The second message, a reminder, would be sent 24 hours before the appointment, reminding the patient that, “... a flu vaccine has been reserved for your appointment.” Thus Milkman and her team found that reminders performed better when they stated a shot was already reserved for the patient and that the messages were congruent with the sort of communications patients expected to receive from their healthcare provider (i.e., not surprising, casual, or interactive).
Overall, these findings show low-cost nudges developed by behavioral scientists, for example text messages sent to patients prior to a primary care visit, can substantially boost vaccination rates. This has to be emphasized: sending text messages comes at almost no cost. The best-performing message, which increased adoption by an estimated 11%, reminded patients twice to get their flu shot at their upcoming appointment. Messaging need not be silly, creative, or interactive – merely to indicate that a shot was reserved and waiting specifically for them. Despite the differences regarding the questions of concern regarding flu and COVID-19 vaccines, this successful script could be used as a template for other campaigns to encourage the adoption of life-saving vaccines against COVID-19, and future vaccines facing similar adoption challenges.
Join us on July 6th at 12 pm EST, for our Webinar - 'The Next Frontier of Healthcare - How BE and digital Technologies Come Together for Better Care'